APOD is a 3-year ethnographic project providing new evidence on the most significant innovation in Western psychiatry and mental healthcare in recent years: a treatment approach called Peer-supported Open Dialogue (POD).
POD is a social network approach to mental distress that places people experiencing severe mental distress and their family and/or others in their network at the centre of treatment. POD is non-diagnostic and shifts the focus of care from treating individual psychopathology to empowering social networks for recovery.
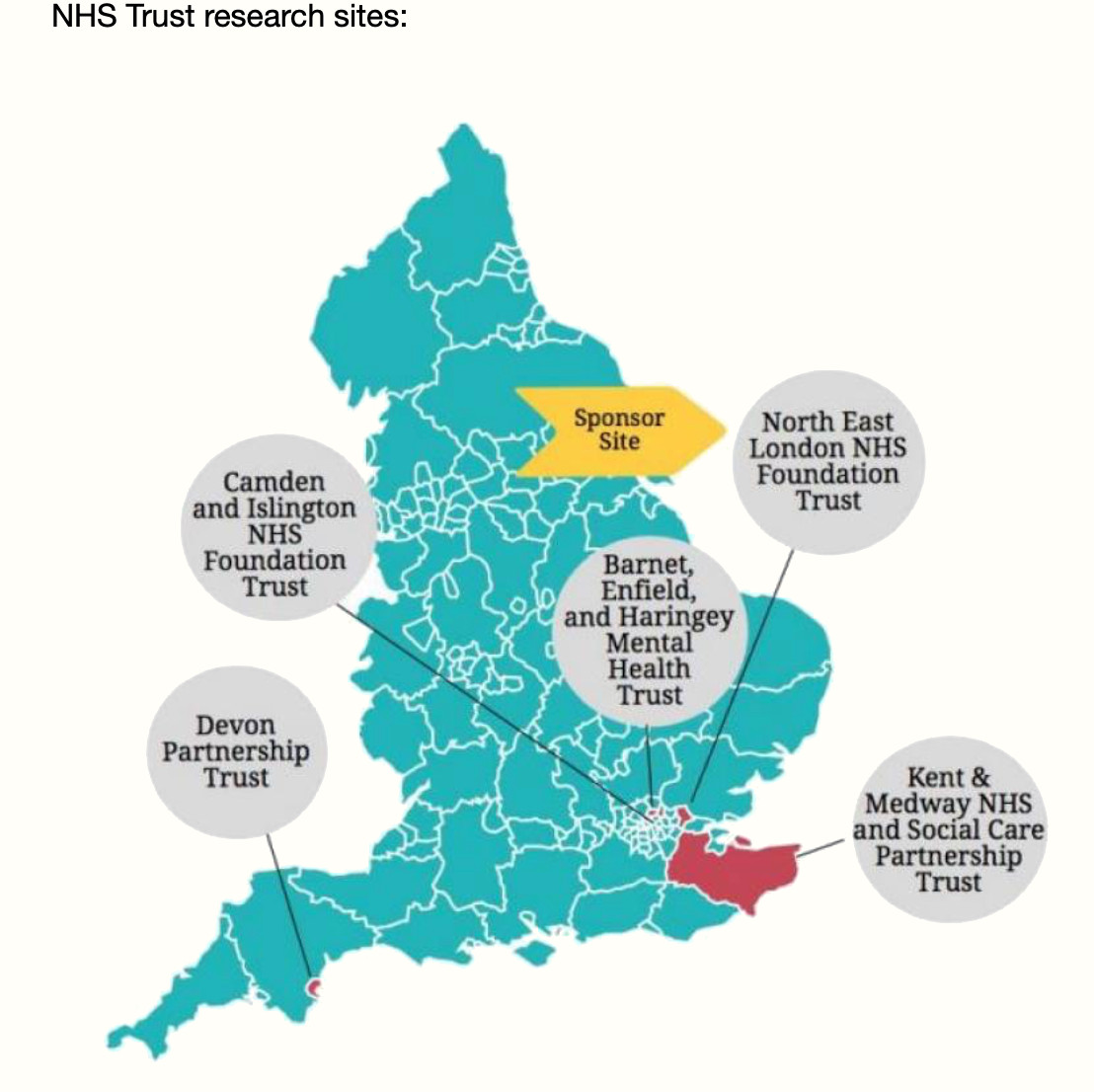
This study is being undertaken alongside the ODDESSI trial (Open Dialogue: Development and Evaluation of a Social Network Intervention for Severe Mental Illness)
The ODDESSI trial compares the outcomes of people in crisis receiving POD with those receiving treatment as usual. The trial will tell us whether on average people in the POD group do better than the treatment as usual group. But it will not explain why or how POD works. The aim of our independent in-depth anthropological study is to better understand the POD approach in practice, and to discover the various factors that influence the success of POD in a given setting. As part of this, we want to understand how POD fits into the wider mental healthcare context of the UK, including advocacy and social movements to improve mental healthcare
What is (Peer supported) Open Dialogue?
Open Dialogue sets out to address some of the most intractable problems in mental healthcare, including long-term dependence on psychoactive drugs, low rates of functional recovery from serious mental illness, over-representation of ethnic minorities in services, and long waiting times. Instead of an expert-led diagnosis-treatment model, OD places clients and members of their social network at the centre of a ‘dialogical’ process aimed at discovering ways out of crisis. At the organisational level, OD ensures rapid response, continuity of care and avoids clinical discussion about clients in their absence (Seikkula & Olson 2003). The OD approach was developed in Finland where studies showed dramatic improvement over treatment as usual for first episode psychosis. Britain’s NHS is now conducting the world’s first randomised controlled trial (RCT) of OD. This large-scale RCT will tell us whether on average people in crisis receiving OD do better across 5 NHS Trust sites; but it will not explain OD, or its wider effects. We are looking at ‘why’ and ‘how’ OD works.
We are conducting a complementary, in-depth ethnographic study to investigate how OD principles are put into practice, the effect of working in this way for families and clinical teams, and the social and contextual factors that shape observed outcomes. The focus is on two NHS Trusts participating in the RCT (in London and Devon) their OD clinical teams, the people who use their services, and their communities. The project will run alongside the RCT for the full 3 years of the trial (2020-2023).
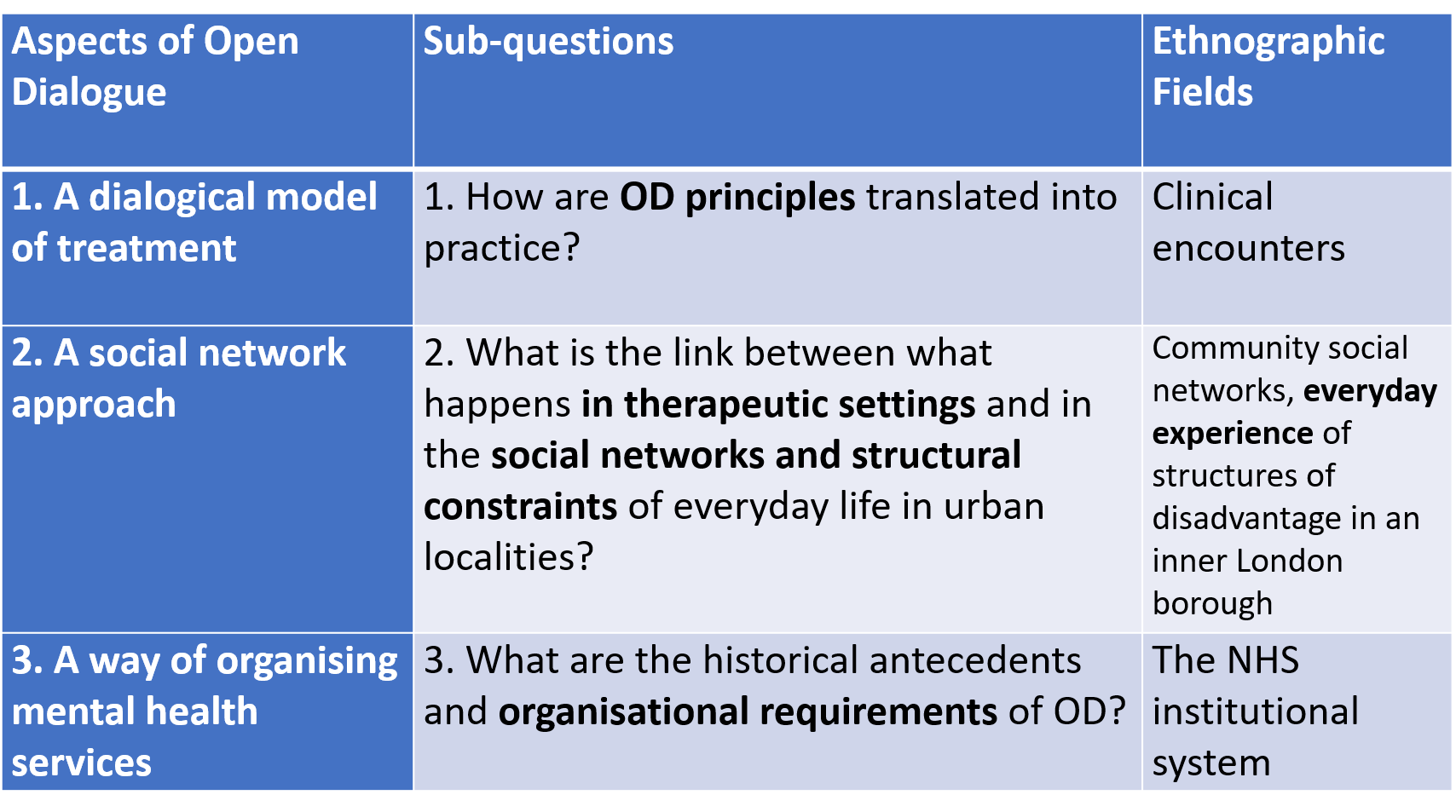
The research carried out by the APOD team will explore three different aspects of OD:
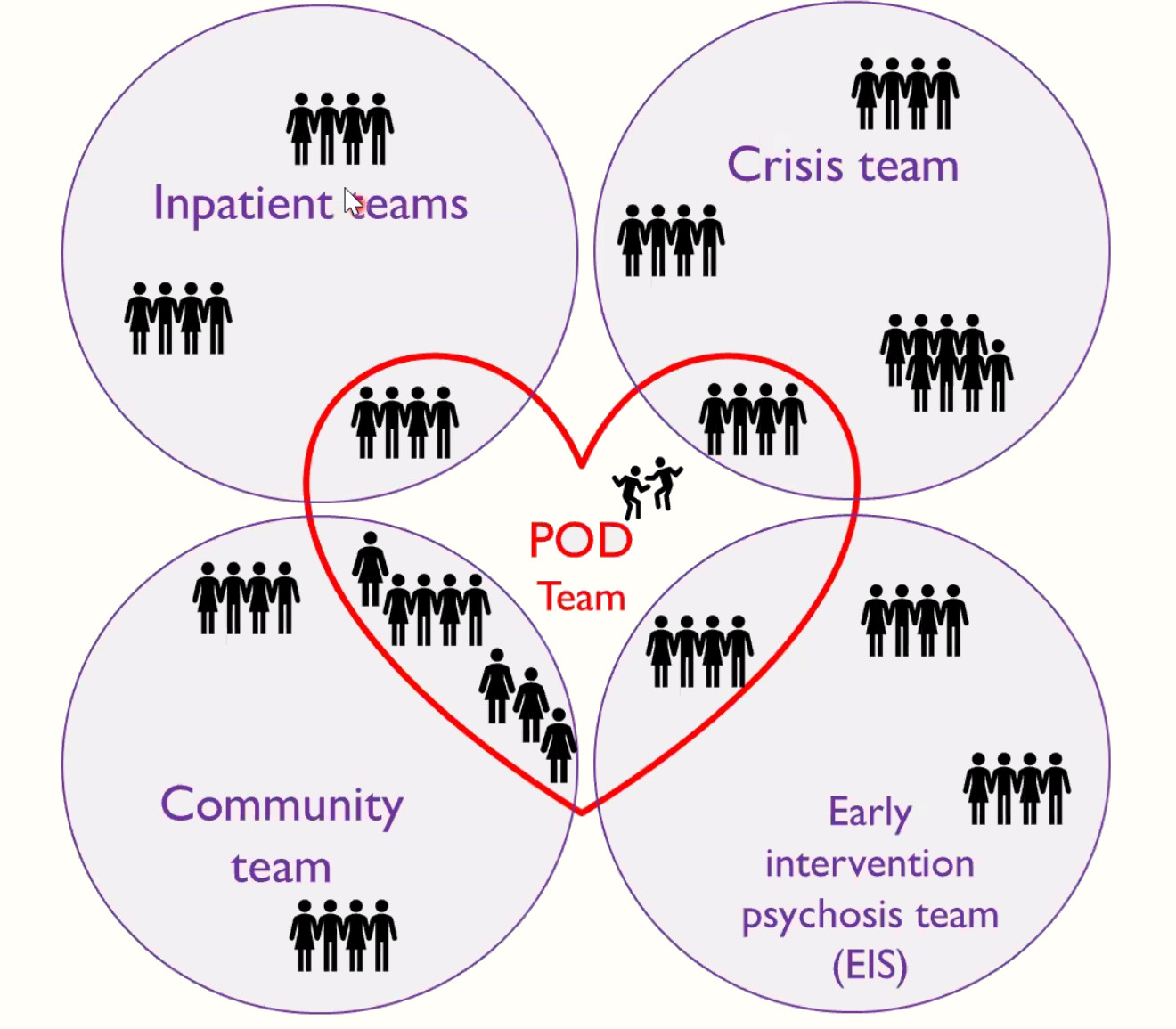
- the dialogical model, studied through immersive fieldwork within Community Mental Health and allied teams (Crisis Resolution, Early Intervention Psychosis) to find out how practitioners translate OD principles into practice within clinical encounters and how this is experienced by clients;
- the social network approach, studied by following the pathway of selected case-study families from the therapeutic OD process into their everyday lives, and by investigating the intersections of professional care networks and community social networks that allow connection and recovery;
- the institutional reorganisation of mental health services instigated by OD, studied through historical research and ethnographic fieldwork. This focuses on how OD teams negotiate new relationships with clients, among themselves, and with the established healthcare system; how OD is adapted to the NHS environment, and maintained as a community of practice. Archival and oral history sources are used to set OD in the context of community psychiatry developed following the closure of large asylums across the UK.
Project findings will enhance the RCT’s policy-relevance and improve the translation of OD into new settings, including, if adopted, across the UK’s NHS. The project also establishes the international OD and Anthropology Network (ODAN), providing a gateway for anthropological insights to shape the development and implementation of OD globally.

What is the purpose of the study?
The purpose of this study is to look at the experience of delivering OD within the context of the ongoing NHS trial in order to better understand the OD approach in practice and to discover the various factors that influence the success of OD in a given setting. The study will produce a detailed descriptive account of the everyday practice and experience of OD. It aims to learn from practice so as to adapt and improve OD and inform its translation into new settings.
Specific aims include:
- To discover how OD principles are translated into practice and how this is experienced by practitioners and clients
- To explore the links between what happens in therapeutic settings and in the social networks of clients’ everyday lives, especially in disadvantaged localities
- To examine the historical antecedents and organisational requirements of OD in the NHS, including institutional barriers to delivering and sustaining the model
- To enable staff practitioners and service users/families to share reflections on their experiences of OD and communicate to wider audiences How will the study be carried out? Ethnographic research generates information on the thing being studied through the direct experience of being part of it. All researchers are themselves trained in OD and participate as practitioners in OD teams. The researchers will obtain consent to observe and take notes on OD clinical meetings and other meetings and events related to OD that they participate in (i.e. ‘participant observation’). In addition, the team will interview practitioners and service users/network members about their experiences. They will also invite staff, service users, and network members to keep reflective journals documenting their experience in their own words.
Conference attended
- ASA 2019 https://theasa.org/downloads/conferences/asa19/ASA19_programme.pdf
- Hope and Dialogue 2020 https://www.hopendialogue.net/wp-content/uploads/2021/10/MIODRC_Book_of_Abstracts.pdf
- Mad in America 2021 https://www.youtube.com/watch?v=NilAfmf7G90
- RAI 2022: Ethnographers as arbiters of truth? Truth and psychiatric systems https://www.therai.org.uk/conferences/mobilising-methods-in-medical-anthropology-2022/programme#10942
Publications
- Mosse, David. (2022). Reflections on Open Dialogue in mental health clinical and ethnographic practice. In Emma Gilberthorpe. (Ed.), Anthropological Perspectives on Global Challenges. (ASA Monograph Series). New York; London: Routledge. https://eprints.soas.ac.uk/37098/